To all those that are practically part fish out there: Yeah, you know who you are. The ones that can't stay away from water. The smell of chlorine gets your blood pumping and you all but grow fins. The water calls to you, beckons sweet nothings. And there you are, jumping in, yelling "Cannonball!" But a few days later, you come into my office complaining of ear pain.
Well, stop it. Stop that water addiction. Your poor ears are ten seconds away from sitting you down for an intervention. But we all know your intense Romeo & Juliet relationship with water, so your ears will just have to suffer. Right? Well, not completely.
So, let's talk about Swimmer's ear: what it is, how to identify it, how to prevent it, and how to treat it.
Often even in medical settings, swimmer's ear, or in expensive medical terms, otitis externa is often mistaken for otitis media, which is an infection behind the tympanic membrane (ear drum) and it is mistakenly treated with oral antibiotics that don't do jack for it. Yep, antibiotics taken by mouth don't do diddly squat to treat it.
Distinguishing Swimmer's Ear from Otitis Media
This is where understanding the difference between the two main types of ear infections comes in handy.
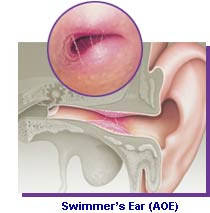
 Otitis externa is an infection that usually presents with a swelling of the external auditory canal which is fancy and again expensive way of stating outside ear canal. Also, it will typically have white, icky gooey gross stuff drain out of it, in a condition called otorrhea, medical jargon for runny ear.
Otitis externa is an infection that usually presents with a swelling of the external auditory canal which is fancy and again expensive way of stating outside ear canal. Also, it will typically have white, icky gooey gross stuff drain out of it, in a condition called otorrhea, medical jargon for runny ear.Another characteristic is that the external auditory canal will often times swell shut, thereby causing a temporary hearing loss.
Fevers may be present but rarely go above 101 degrees Farenheit (38.3 degrees Celsius).
Other characteristics: Most common in the summer. Recent swimming. Pain is achieved by pulling on the ear.
Otitis media is an infection with fluid and pus behind the ear drum. The condition occurs most commonly in winter months and is associated with a recent upper respiratory infection. Has a runny nose then think more otitis media. Children with it will often act more restless at night.
As far as drainage, the pus typically doesn't drain out the ear unless there is a perforation of the tympanic membrane. This occurs when the pressure behind the eardrum becomes so great that the membrane blows open like a pair of briefs after a burrito binge-fest, thus letting the pus go pouring out screaming "free at last!"
But under normal circumstances, there is no drainage from the ear, unlike in otitis externa which runs a marathon.
Fevers are present the majority of the time and are often times greater than 101 degrees F (or greater than 38.3 degrees C)
In addition to fevers, sufferers of otitis media most commonly have a dense loss of hearing that feels similar to trying to hear while under water.
Hearing loss can be up to 30 decibels is more commonly seen in otitis media than in Swimmer's ear... because normally, otitis media doesn't drain, which is why one of the main treatments for chronic otitis media is to place tubes in the ear drums. (Note: otitis externa can cause hearing loss if the canal is occluded due to increased swelling.)
Speaking of drainage from the ear, the type of otorrhea can actually help you in diagnosing what type of ear infection or injury you have. Yeah, I know what you are thinking: "Ewe, I don't want to know more about diarrhea from the ear!" But come on, you know you're curious. It's like the trainwreck that you just can't help staring at. It has that so gross but so addicting thing about it. Pretty soon, you're going to start looking in people's ears, searching for waxy treasure and loving every minute of it.
So here it goes: The low down and dirty of ear drainage.
Otitis Externa
- Acute Bacterial --- Scant white mucus (yummy) but can be thick and juicy
- Chronic Bacterial --- Bloody drainage
- Fungal --- Fluffy and white like a kitten. But can be black, or bluish-green. Ahh, it's colorful.
- Acute --- Yellow to white pus with Pain
- Chronic --- More Pus but without Pain
- Cerebral Spinal Fluid Leak --- Clear, watery
- Bony Trauma --- Bloody mucus
So before I get too technical, I might as well show you the anatomy of the ear. I'm only doing this for you. I, personally, really didn't like anatomy. I smelt like formaldehyde after each class. Parfume a' la cadaver bodies. Not good for the social life, so I'm a little bitter. But for you, I'll make an anatomy exception.
There. That's my extent of giving you anatomy. Feel the love. Okay now, moving on.
Causes
- Swimming
- High humidity
- Higher outside temperatures (a.k.a summer)
- Sweating
- Water contaminated with bacteria (okay, all water is "contaminated" with bacteria unless it comes to you in a sealed bottle stamped "Sterile.")
- Sticking stuff in your ears like Q-tips, keys, toys, unlucky rabbit's feet, etc.
Otitis externa presents like you've been kicked in the ear. The American Academy of Family Physicians states that the most common symptom is ear discomfort. But come on. How many of you mer-people will actually jump out of the water long enough to go to the doctor's office for "ear discomfort."
Yeah, that's right. I see you in my office when you're screaming and crying, wailing and gnashing of teeth, because it hurts like a freaking sea horse kicked you in the ear... correction an itcy seahorse. Did I forget to mention the intense itching? Or pruritis, if you want to be technical. Itching = $5 word. Pruritis = $5,000 word. Doctors like to use the $5,000 word: it pays for our yachts, or in my case, my beaten up RV.
So, in a nutshell: Ear discomfort (otalgia, another $5,000 word), which worsens with touching the ear or chewing, and ear drainage (otorrhea. Again, Cha-ching!). A bad case of swimmers ear can be so intense with pain though that the a patient may require analgesics. Patients may also complain of ear "fullness" and/or hearing loss due to the swelling of ear canal until it occludes the opening.
Prevention
Stay out of the water. Okay, that's not going to work. That's about as useless as saying to a room full of drug addicts: don't take this crack that I'm leaving here on the table in front of you, because it's bad for you.
Dry Your Ears
Next option, is to dry your ears after water immersion. Using a blowdryer to gently dry your ears is actually quite affective in preventing Swimmer's ear. The excess moisture in your ear, removes the natural protection of your ear's waxy secretions and thus increases the pH in the canal. This provides the optimal environment for growing bacteria and thus leads to infection. The most common bacteria that infect the outer ear canal are Pseudomonas aeruginosa and Staphylococcus aureus.
Acidify the Canal
Yep, you heard me right. The natural environment of the external auditory canal is relatively acidic around a pH of 4.5 compared to the body's internal pH which is 7.4. This acidic environment protects the canal under normal circumstances from infection with bacteria. (For more information: Read the article "Change of External Canal pH in Acute Otitis Externa published by the Annals of Otology, Rhinology and Laryngology http://www.ncbi.nlm.nih.gov/pubmed/19999361)
- Mix one part alcohol (rubbing alcohol, not beer) with one part white vinegar.
 Put Nothing in Your Ears
Put Nothing in Your EarsMy boss, Dr. Tacket is quoted to say, "Put nothing but your elbow in your ear."
So literally, it means put nothing in there. No Q-tips, no keys, no bobby pins, no fingers, no toys, no bugs, no nada. Nothing. Zippo. One, you can damage the external auditory canal, making it much more susceptible to infection. Two, you push the ear wax down towards the tympanic membrane where it can get lodged and cause cerumen impaction, which results in a reduction of hearing. And three, I seriously don't want to dig out that junk out of your ears. It exhausts me. Granted, digging cockroaches and beetles out of people's ears exhausts me more, because I have to fight my gagging reflex the whole time and end up paranoid for weeks about a bug climbing into my own ear. Not fun, I tell you. Not fun.
Keep Ears Dry
Then don't allow water in your ears. Where good fitting ear plugs while bathing or in the water. A cheap way of preventing water getting in your ears while showering is to put a cotton ball in your ear with vaseline on it (on the side of it facing outward). This acts as a water barrier. Then immediately remove the cotton balls or ear plugs from your ears once you are out of the water.
I know, I know. I just said don't put anything in your ears. Well, ears plugs and temporary cottonballs dipped in Vaseline don't count.
Treatment
This is the interesting part. As with all things, the treatment varies according to severity of condition. But there are some straightforward ground rules:
- Oral antibiotics don't work for swimmer's ear at all, period. They only work if otitis media is involved due to perforation. But that's otitis media.
- The antibiotics that are useful are in ear drops or even eye drops.
- The antibiotics must come in direct contact with the bacteria on the surface of the ear canal for them to work.
- If the ear canal is swelled shut, you have to force a wick into it, which is a painful process, and then drop the ear drops onto the wick.
- You need certain instruments available that you can clean the infection debris out of the ear with.
- Six, never, never, never under any circumstances flush the ear with water or get water into the ear. Makes the situation worse like throwing gasoline onto an oil fire.
- Seven, oral antibiotics don't treat otitis externa.
The main treatment of otitis externa is topical. If the external auditory canal is not occluded, place antibiotic drops in the ear canal itself.
Some of the topical solutions out there, according to the American Academy of Family Physicians include the following (The brand name will be in paretheticals):
Pharmaceutical Acetic solutions (or you can use the homemade alcohol/vinegar solution)
- 2% acetic acid solution (VoSol) $49
- 2% acetic acid with hydrocortisone (VoSol HC otitic) $59
- 2% acetic acid with aluminum acetate (Otic Domoboro) $18
- Neomycin with polymyxin B-ydrocortisone (Cotisporin) $42
- Ofloxacin 0.3% solution (Floxin Otic) $34
- Ciprofloxacin 0.3% with hydrocortisone suspension (Cipro HC Otitic) $59
- Ofloxacin 0.3% (Ocuflox) $29
- Ciprofloxacin 0.3% (Ciloxan) $30
- Gentamicin 0.3%
- Tobramycin 0.3%
Push the tragus (that small flappy thing that everyone asks why is that thing there in front of your ear canal) in a few times after administering the drops in order to further distribute the antibiotics within the ear canal.
The symptoms should start to cease after 3 days. If the symptoms don't stop than the external auditory canal is most likely swollen shut and the antibiotics aren't reaching the infected skin.
Insert wick using an otoscope (or you can use a headlight strapped to your forehead and a magnifying glass) into the infected ear canal. It will hurt the patient terribly, so be prepared to be beaten. Give the patient pain killer before proceeding.
Ear wicks are made by several different companies, namely Otocell and Americell brands. After inserting the wick, then apply the ear drops to it.
If a wick is required than the drops should be applied every 3 to 4 hours while patient is awake. After a few days (2 to 5 days), pull the wick out and reexamine the ear canal. Redo this process every 2 to 5 days until the swelling of the canal is resolved and the wick is no longer needed.
If there is an ear drum perforation, the only drops that you can use are ofloxacin (Floxin Otic) drops.
For more information, please refer to:
J. David Osguthorpe, MD and David R. Nielsen, MD. (2006). "Otitis Externa: Review and Clinical Update," American Family Physician, 74, pp. 1510-1516.
Robert Sander, MD. (2001). "Otitis Externa: A Practical Guide to Treatment and Prevention," American Family Physician, 65, pp. 927-936.
Anyway, thanks for reading. TTFN
Dr. Princeton, D.O.
Edit Note:
In terms of barotrauma of the ear, or trauma due to changes in pressure:
The pain associated starts during a descent of a plane or while scuba diving. Blood may or may not appear behind the tympanic membrane. If there is blood, then this is called either a tympanic membrane hemorrhage or a serous/hemorrhagic middle ear fluid expression. About 10 percent of adults can get barotrauma after a regular flight, making this a very common occurance.